SAN ANTONIO — If you or a loved one is in immediate danger, call 9-1-1. If you are in a moment of crisis and need someone to talk to, you can call the National Suicide Prevention Hotline at 1-800-273-TALK or text the Crisis Text Line at 741-741. You can also find a web-based chat service here. You may want to consider adding these numbers to your phone in case you ever need them in the moment.
If you've ever been concerned about a family member or friend's mental health, you may have wondered about the best way to provide support. Dr. David Roberts, Director of UT Health San Antonio Transitional Care Clinic, says taking action can make all the difference.
"Social connectedness is a huge factor," Roberts said. "If you talk to people that have experienced suicidal thoughts or attempted suicide and gotten through it, social support is something they point to as one of
the big factors that gets them through. Very often it can be just small moments, small gestures; 'so-and-so reached out to me, I thought I was in a dark hole by myself and just her reaching out to me made all the difference.'"
Claudia Vargas, a peer policy fellow with the Hogg Foundation who works with groups such as the National Alliance on Mental Illness and SA Clubhouse, a space for mental health recovery, says everyone has mental health, so anyone can have a mental health condition. As someone who's experienced suicidal thoughts and has gotten help, she now advocates for others.
KENS 5 Eyewitness News asked Roberts and Vargas to weigh in on their thoughts about how we can support our friends and family members.
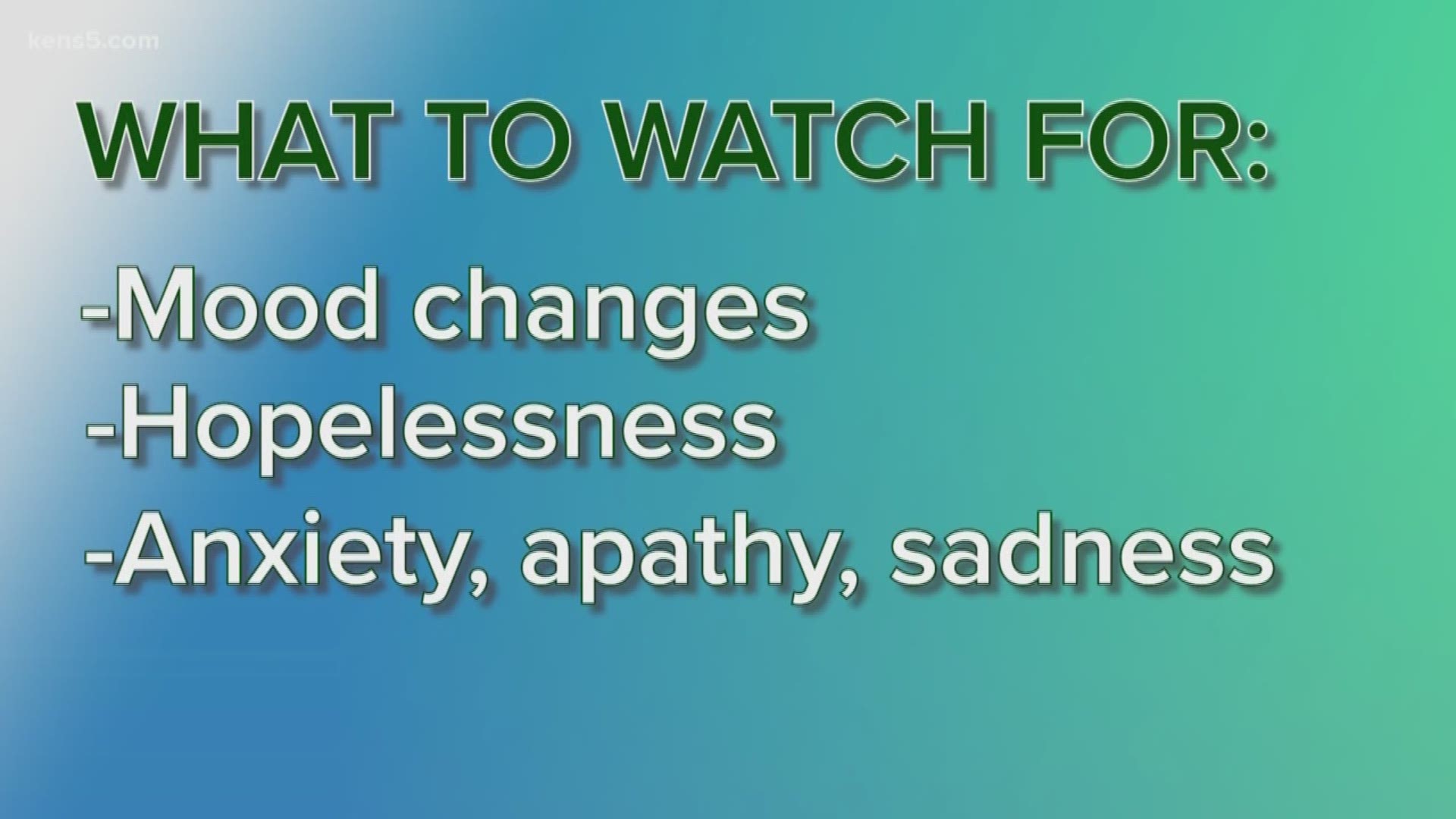
WHAT TO WATCH FOR
Roberts: There’s different ways clinicians and researchers try to assess the risk of suicide. Very few people luckily actually attempt suicide, so the risk factors that are out there- even if someone has these risk factors, there’s still a low chance they’ll commit suicide- but still there are some that are important.
Obviously if they’re experiencing depression, if they have a history of attempting suicide, if they’ve had people in their lives that have attempted or committed suicide, if they’re using drugs or alcohol at a higher risk than they normally do, if they are prone to impulsive behavior, and experiencing any recent loss or disappointment, all of these combined in any sort of combination can be an indicator that someone might be at risk.
Other factors could be withdrawal or saying statements like “I feel worthless,” or making statements like they don’t see a future for themselves. Listening to the words they use can be very helpful as well.
Vargas: I think in general, if somebody is distancing themselves or they seem not like their usual self go ahead and have those kinds of conversations: hey, how are you doing? Is there something that’s bothering you, how can I help?
I think everybody is susceptible to having a mental health [crisis]. Everybody has mental health, so anybody can have a mental health condition. There are definitely people that are the spirit of the room, always laughing and cracking jokes- but they can be going through a crisis themselves.
STARTING A CONVERSATION
Roberts: Oftentimes if you’re feeling concerned about a family member or a friend, you’ve seen something or heard something that’s different from the way they usually are and you’re worried about their safety, if you’re worried about depression or suicide. I think the best thing to do if possible is to actually refer to something concrete. Say something like- last week I saw you say, my life is useless. Using that concrete thing to refer to is really helpful and shows them you’re paying attention and prevents them from saying, “it’s nothing at all.” And then you can say your concerns about that. “I heard you say your life is useless- I wonder if you’re thinking about hurting yourself, or killing yourself.”
One of the most important things to make known publicly: there’s this idea that if I ask somebody about suicide, will that put the idea in their head or make them think, oh I should commit suicide- or make them horrified that I would even bring that up. One of the most important things we can do is be comfortable bringing up the question of the suicide. There’s very clear research out there that bringing it up does not at all increase the risk of suicide. In fact, there’s some evidence it’s the opposite. For people thinking about suicide, often they feel ashamed and alone and alienated- like they can’t talk with other people about it. By bringing it up and asking them about suicide, they feel like they have somebody to talk about it.
The most important one is- bring it up with them, in a direct way and in a caring way. I think one thing I would like to be sure people understand is- talking about safety and suicide is very important for friends and loved ones. We want to keep people safe if they’re at risk for suicide. But people who are at risk for suicide- their goal very often is not to stay safe, it’s actually to suffer less. And the research shows clearly that people who are at risk for suicide are trying to stop pain, to escape emotional pain or physical pain- so talking with loved ones about the pain they’re in, validating their suffering and not talking to them in a way that communicates they may be trying to manipulate or get attention – that’s one misconception, when someone is talking about dying, sometimes we think they’re trying to get attention for that- the research doesn’t really support that. Show them that we care and ask if we can help them in any way to reduce the pain.
Vargas: It comes down to intention. You have to be careful about your tone and how you approach it. You don’t just go in front of a big group – hey, are you doing okay? Just make sure it’s in private and you ask them if they’re doing well. Sometimes during family holidays people ask, do you have a partner or how’s school doing and maybe that’s a touchy subject for you at the moment. Just be more careful about the words and tone that you use when asking people how they’re doing.
I think people are scared either to push too far or be too straightforward about certain topics, like suicide. Some people are told and they believe wrongfully that asking, hey, are you feeling suicidal? That if they weren’t already feeling suicidal, they might go ahead and complete suicide. But it’s quite the opposite. If you ask someone- hey I feel like you’ve been off lately, and you mentioned things like, I don’t find purpose in life anymore- key words that would tell you someone’s thinking about suicide- you want to make sure you ask them. Are you thinking about suicide? And can I help you? Because talking about it takes away that stigma and that barrier of talking about it. Just asking will lead to a more since conversation that will lead to more positive results long term.
If they say yes, there are various ways you can go about it. Somebody may be thinking about suicide, but not actively planning to die by suicide. So you want to ask- do they have a plan? Are they thinking about hurting themselves in the next 24 hours? That’s from the crisis counselor background. You mostly just want to listen to whatever’s going on, not try to solve the problem- because if you’re having suicidal thoughts, chances are one conversation isn’t going to make it go away. Listening, and if you know- say hey, here’s the crisis text line number, or- I’m here for you. How can I be here for you- leaving it open ended for that person to help.
CREATING A "SAFETY," WELLNESS OR "CRISIS RESPONSE PLAN"
Roberts: They’re used in clinical settings but more and more research shows friends and family members can be helpful doing a suicide safety plan with people. We’ve actually started thinking about it as a form of mental health first aid. In the same way that you don’t have to be a doctor to do CPR, you don’t have to be a doctor to do first aid for someone feeling suicidal. The term “suicide safety plan” may not be the best term to use, because it sort of implies the person having suicidal thoughts has the goal of being same. But almost by definition- if they’re feeling suicidal, they’re not focused on being safe. What they’re focused on is stopping the emotional suffering or physical suffering, the pain they’re in. So when you’re making a plan- try crisis response plan. It’s a list for the person that shows, what are your personal risk factors? What are the things that give you a sign you’re getting to a crisis stage, where the pain is going to be intolerable. The second thing, is what can you do by yourself to lessen the pain you’re in? Three- what can you do to reach out to people for social support? Four, what are the things that have been meaningful to you in the past? Helping the person get in touch with what matters to them in life- pets, children, family, those kinds of things. And finally, emergency resources. When all of these things have not helped you to lessen the pain- can you call 911, can you go to the hospital?
These are helpful because often when someone is suicidal- they get blinders on. We aren’t thinking reflexively, we can’t solve problems well, our thinking gets rigid, dark and present focused. What this does is help them in the moment. They can take a picture of this with their smartphone and when they’re feeling suicidal, and can’t think straight- they pull out their crisis response plans, follow the directions, and it gets them through.
Vargas: WRAP is a Wellness Recovery Action Plan. You sit down with a book and it asks you a whole bunch of questions about- what do you need to do to be well? Or, what are some signs that you’re not doing so well? So you can catch yourself and say- maybe it’s been more of a struggle to get up from bed in the last couple weeks. A pre-crisis moment. And you make a list of, when you are in those moments- what are things you can do? Who are people you can reach out to, it also goes over, if you’re going through a crisis, who’s going to help you? Who do you want to contact, who do you not want to contact? So you already have a plan and can be calm in the moment. (In San Antonio, The Clubhouse offers free classes for how to fill out a form).
This is for anybody. You don’t have to technically be diagnosed and have a mental health condition- but if you have mental health, chances are a plan will be helpful for you. It will be beneficial to you- and those around you.
OTHER HELPFUL RESOURCES:
Do you have a suggested resource for us to add to this list? Contact ezucco@kens5.com.